Tiếng Anh Sản Phụ Khoa – HungVuong ME.Class
CERVICAL CANCER
Vocabulary
Reading 1: What you need to know about cervical cancer
Reading 2: Modern Treatment of Cervical Cancer
Grammar notes: Noun Phrase and Verb Phrase
A case report: Cervical cancer
Vocabulary
- Uterus: the uterus or womb is a major female hormone-responsive secondary sex organ of the reproductive system in humans and most other mammals.
- Tumor: a tumor is a mass of tissue that’s formed by an accumulation of abnormal cells. normally, the cells in your body age, die, and are replaced by new cells.
- Cancer: Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.
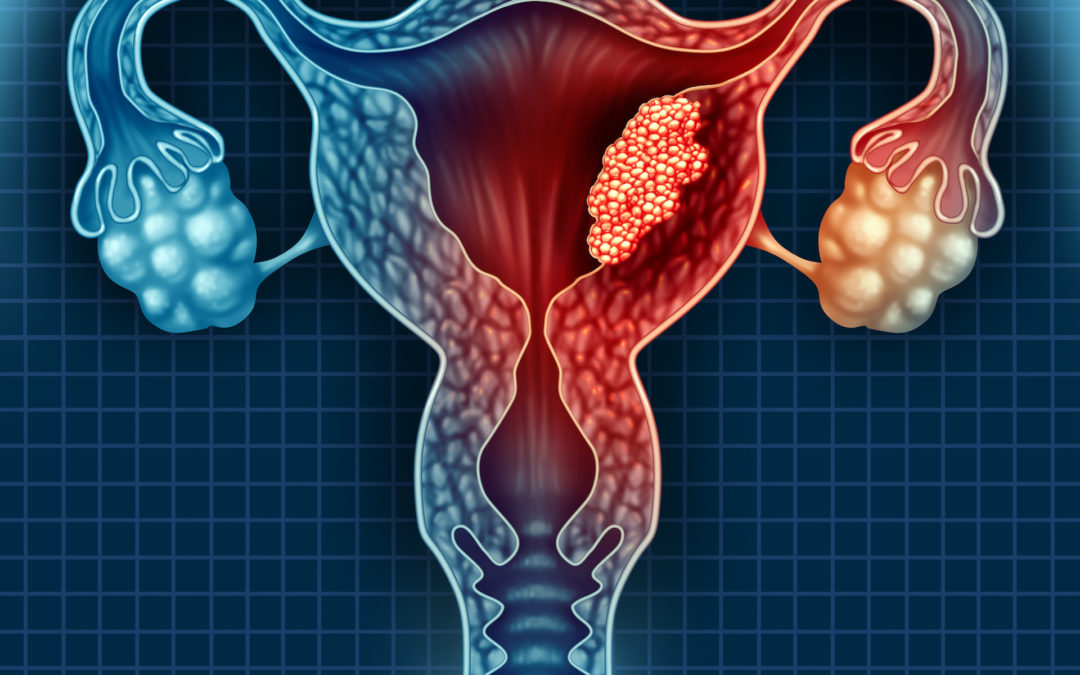
- Cervical cancer: Cervical cancer is a cancer arising from the cervix. It is due to the abnormal growth of cells that have the ability to invade or spread to other parts of the body.
- Papilloma: A papilloma (plural papillomas or papillomata) (papillo- + -oma) is a benign epithelial tumor[1] growing exophytically (outwardly projecting) in nipple-like and often finger-like fronds. In this context, papilla refers to the projection created by the tumor, not a tumor on an already existing papilla
- Human papilloma infection: Human papillomavirus infection (HPV infection) is an infection caused by the human papillomavirus (HPV)
- Vaccine: A vaccine is a biological preparation that provides active acquired immunity to a particular disease.
- Menstruation: Menstruation, also known as a period or monthly,[1] is the regular discharge of blood and mucosal tissue (known as menses) from the inner lining of the uterus through the vagina
- Period: menstruation
- Vaginal discharge: Vaginal discharge is most often a normal and regular occurrence. However, there are certain types of discharge that can indicate an infection. Abnormal discharge may be yellow or green, chunky in consistency, or foul smelling. Yeast or a bacterial infection usually causes abnormal discharge.
- Leukorrhea: Leukorrhea or (leucorrhoea British English) is a thick, whitish or yellowish vaginal discharge.
- Postcoital pain: Dyspareunia. Dyspareunia is painful sexual intercourse due to medical or psychological causes.
- Cone biopsy: A cone biopsy is an extensive form of a cervical biopsy. It is called a cone biopsy because a cone-shaped wedge of tissue is removed from the cervix and examined under a microscope.
- Radical hysterectomy: Radical hysterectomy refers to the excision of the uterus en bloc with the parametrium (ie, round, broad, cardinal, and uterosacral ligaments) and the upper one-third to one-half of the vagina.
- Radiotherapy: Radiation therapy (also called radiotherapy) is a cancer treatment that uses high doses of radiation to kill cancer cells and shrink tumors.
- Chemotherapy: Chemotherapy is a drug treatment that uses powerful chemicals to kill fast-growing cells in your body. Chemotherapy is most often used to treat cancer, since cancer cells grow and multiply much more quickly than most cells in the body. Many different chemotherapy drugs are available.
- Chemoradiation: Chemoradiation is a combination of chemotherapy and radiotherapy. It is also sometimes called chemoradiotherapy. Chemoradiation may be given: before surgery, to help shrink the cancer and reduce the risk of cancer coming back in or around the rectum.
- Brachytherapy: Brachytherapy is a form of radiotherapy where a sealed radiation source is placed inside or next to the area requiring treatment.
Reading 1
What you need to know about cervical cancer
Cervical cancer affects the entrance to the womb. The cervix is the narrow part of the lower uterus, often referred to as the neck of the womb.
The American Cancer Society estimates that doctors will make 13,170 new diagnoses of cervical cancer by the end of 2019 in the United States. More than 4,200 women in the U.S. will die from cervical cancer this year.
Human papillomavirus (HPV) causes the majority of cervical cancer cases. The HPV vaccine successfully prevents HPV.
The Centers for Disease Control and Prevention (CDC) initially recommended the vaccine for all people aged 9–26 years. However, the CDC now advise that the vaccine is also available for all women and men aged 26–45 years who did receive the vaccine as a preteen.
In the early stages of cervical cancer, a person may experience no symptoms at all. As a result, women should have regular cervical smear tests, or Pap tests. A Pap test is preventive. It aims not to detect cancer but to reveal any cell changes that indicate the possible development of cancer so that a person can take early action to treat it.
The most common symptoms of cervical cancer are:
- bleeding between periods
- bleeding after sexual intercourse
- bleeding in post-menopausal women
- discomfort during sexual intercourse
- vaginal discharge with a strong odor
- vaginal discharge tinged with blood
- pelvic pain
These symptoms can have other causes, including infection. Anyone who experiences any of these symptoms should see a doctor.
Extracted from: https://www.medicalnewstoday.com/articles/159821.php#stages
Reading 2
Modern Treatment of Cervical Cancer
The treatment of cervical cancer is dictated by International Federation of Gynecology and Obstetrics (FIGO) stage, which is a clinical staging system. For patients with early cervical cancers, surgery is recommended. A cone biopsy is adequate treatment for patients with stage IA1 disease, whereas for patients with stage IA1 disease with lymphovascular space invasion or stage IA2 disease, a cone biopsy with negative surgical margins and pelvic lymph node dissection are recommended. Fertility‐sparing surgery is an option for patients with early‐stage cervical cancers. For patients with high‐risk stage IA1 through stage IB1 disease, a radical trachelectomy and pelvic lymph node dissection can be considered. An additional option for some patients would be pelvic radiotherapy and brachytherapy. There currently are ongoing trials evaluating reduced‐intensity surgery for patients with early‐stage lesions. The Simple Hysterectomy and Pelvic node dissection in Early cervix cancer (SHAPE) trial is evaluating simple versus radical hysterectomy for patients with cervical tumors measuring <2 cm in size. SHAPE is a CCRN trial that has immediate application to underresourced countries. A randomized trial of surgery versus radiotherapy for patients with stage IB1 to stage IIA cervical cancer demonstrated no difference in survival. It is interesting to note that patients in this trial did not receive chemotherapy, and 84% of patients in the surgical arm with tumors measuring >4 cm required postoperative radiotherapy. Morbidity was noted to be greater in patients who received both modalities, and therefore current recommendations are to try to use a single modality.
Advanced imaging such as computed tomography, magnetic resonance imaging, and positron emission tomography are not permissible in FIGO staging; however, imaging (if available) should be used to appropriately guide treatment. Positron emission tomography scans are helpful for delineating the extent of disease. Magnetic resonance imaging is superior at demonstrating soft tissue resolution for the extent of cervical cancer within the pelvis. This can be critical for brachytherapy treatment planning or conformal radiotherapy techniques.
A National Cancer Institute Alert in 1999 demonstrated the superiority of cisplatin‐containing concurrent chemoradiotherapy for women with advanced cervical cancer. The hazard rate for reduction and death was approximately 0.52. Consequently, this technique was rapidly adopted worldwide, and weekly cisplatin became the worldwide standard. The optimization of chemotherapy is unclear, and the CCRN has 3 trials testing the optimal combination of chemotherapy and radiotherapy. Extended adjuvant chemotherapy in patients with locally advanced disease currently is being tested in the OUTBACK (A Phase III trial of adjuvant chemotherapy following chemoradiation as primary treatment for locally advanced cervical cancer compared to chemoradiation alone) trial. The Radiation Therapy Oncology Group (RTOG) 0724 trial also is evaluating extended adjuvant chemotherapy for patients treated with a radical hysterectomy who have positive lymph nodes or positive parametria, although this currently is not a CCRN trial. Dose‐intense neoadjuvant chemotherapy is being tested in the phase 3 INTERLACE (A phase III multicentre trial of weekly induction chemotherapy followed by standard chemoradiation versus standard chemoradiation alone in patients with locally advanced cervical cancer) trial. In addition, a phase 2 trial showed promising results with a higher dose of cisplatin administered every 3 weeks. This finding now is being compared with weekly cisplatin in the Tri‐weekly Administration of Cisplatin in Locally Advanced Cervical Cancer (TACO) trial. The TACO trial has been the most successful CCRN trial, with significant accrual from Vietnam and Thailand.
In patients with advanced disease who are receiving curative radiotherapy, an important quality metric is to keep the total treatment course duration within 8 weeks. In multiple studies, prolonged treatment after 8 weeks has been shown to have an approximate 1% loss in local control for every day of treatment beyond 8 weeks. Adherence to a few quality metrics such as receipt of concurrent chemoradiotherapy, brachytherapy, and completion of treatment within 8 weeks will markedly improve survival worldwide.
Extracted from: Cervical cancer – A global health crisis
https://onlinelibrary.wiley.com/doi/full/10.1002/cncr.30667
Grammar note (*)
CASE REPORT
A 50-year-old G5 P5 woman complains of postcoital spotting over the past 6 months. Most recently, she complains of a malodorous vaginal discharge. She states that she has had syphilis in the past. Her deliveries were all vaginal and uncomplicated. She has smoked 1 pack per day for 20 years. On examination, her blood pressure (BP) is 100/80 mm Hg, temperature is 99°F (37.2°C), and heart rate (HR) 80 is beats per minute (bpm). Her heart and lung examinations are within normal limits. The abdomen reveals no masses, ascites, or tenderness. Her back examination is unremarkable and there is no costovertebral angle tenderness. The pelvic examination reveals normal external female genitalia. The speculum examination reveals a 3-cm exophytic lesion on the anterior lip of the cervix. No other masses are palpated.
What is the most likely diagnosis?
What is your next step?
Extracted from: Obstetrics and Gynecology Casefile, 3rd edition
DOWNLOAD THIS LESSON:
DR.NGUYỄN THÁI DUY
Để lại một phản hồi Hủy